 Unlocking the Potential to Transformational Change
Unlocking the Potential to Transformational Change
It’s rare to pick up an article on the rapid pace of change in health care today without encountering the word “collaboration.” As healthcare reform unfolds and incentives for reimbursement shift from fee-for-service (do-more-get-more) to one that reimburses for keeping patients healthy (value-based payments), the need to collaborate across departmental, organizational, sector, and community boundaries has emerged in healthcare as never before.
Collaboration involves working across professional boundaries, engaging in joint decision making and sharing ownership of decisions. Here are just a few examples of the shift from competition (or at best coordination) to collaboration across boundaries in healthcare:
 Payers and providers who for decades related primarily through negotiation and competition are recognizing collaboration is an effective route to improving care delivery.[1] At the forefront are hospital networks with health insurance companies and health insurers who are running hospitals to deliver higher quality, value-based care.[2]
Payers and providers who for decades related primarily through negotiation and competition are recognizing collaboration is an effective route to improving care delivery.[1] At the forefront are hospital networks with health insurance companies and health insurers who are running hospitals to deliver higher quality, value-based care.[2]- Rural and large urban hospitals are partnering to consolidate and deliver care.
- The Institute of Medicine recommended that nurses, physicians and other health professionals be full partners in working together to redesign healthcare.[3]
- Public health departments and hospitals are seeking ways to assess community needs and collaboratively develop community health improvement plans.
At the same time, it’s an uphill process. Until recently, collaboration across the spectrum of healthcare has not been highly valued, so few healthcare leaders “grew up” in a collaborative context. “Collaboration needs a different kind of leadership; it needs leaders who can safeguard the process, facilitate interaction and patiently deal with high levels of frustration.”[4]
In other words, since feelings are the drivers or barriers to collaboration, this way of engaging requires emotional intelligence (EQ). As the precursor of collaboration, emotional intelligence is the ability to blend thinking, feeling and acting for optimal decisions. This requires tuning into emotional data, responding intentionally, and using the opportunity to move forward meaningfully.[5]
Certainly, collaboration includes technical and intellectual skills – yet neuroscience shows that collaborating with people is governed by emotion. That’s why working together can be delightfully invigorating or profoundly threatening.
Competing Neural Pathways
Emotional intelligence may be key to collaboration because of two parallel neural pathways that are triggered when two parties sit down to work together (or not).
First let’s look at the bright side. When collaboration goes well, research demonstrates that oxytocin is released. This feel-good-because-you’re-connecting neuro-hormone is released when our thoughts, feelings and actions blend with others. This is the same chemical that is released when a new mother looks into the face of her child, when we pet the dog or cat – or when the team is flowing in synch, like a glorious ballet.
On the other hand, as David Rock points out in Your Brain at Work, when we perceive someone as a competitor or adversary, empathy and oxytocin plummet along with our willingness to explore the validity of other’s ideas, or even hear their ideas.[6] When we evaluate the other person as a threat, a primal stress response is triggered. We put up walls and sharpen our axes.
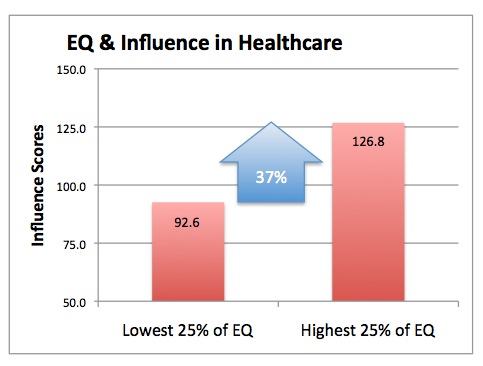
Influence is a key component of collaboration. Research with the Six Seconds Emotional Intelligence Assessment (SEI) on 321 healthcare professionals shows a very strong link between EQ and influence. Those with higher EQ scores also had a 37% advantage on influence.[8]
So, imagine a provider and third party payer are coming together to work on creative solutions for keeping an entire population of patients healthy. For decades their relationship has been characterized by competing commitments and acrimonious negotiations. They’ve been told they have to collaborate – but when they sit down across the table from one another, loaded with decades of defensiveness, are we going to see a ballet or a battle?
The Foundation of Collaboration
It’s easy to say, “we need collaboration,” but if we don’t attend to the underlying emotional requirements, it’s unlikely at best. One key step is building connection. The parties need to FEEL that they have a shared purpose – that they’re on the same team. This is easy to say, but given our history in healthcare, it’s difficult to achieve. Here are three tips when working to shift toward the new frontier of collaboration:
1. Build in time for personal connection. When we meet across the table wearing our roles, we carry our history and thus may automatically scan for threats. When we first create connection through getting to know the person we find that all these people are actually human beings. Through building a personal relationship, a new door opens.
This time is not just “nice to have experienced,” nor is it “wasting time before we get to the real work.” It’s essential ground-breaking – without which, the foundations will be unstable.
2. Choose your emotions. Consider how you want to feel, and how you want others to feel, at the end of each meeting. Pay attention to your emotions and the emotions of others. Noticing and silently naming your emotions can be a powerful way to stay present and move from defensiveness to openness.
3. Engage optimism. An optimistic perspective increases hope, broadens possibilities and supports innovative thinking. Focusing on solutions and desired outcomes, even in the face of significant challenges, helps you see beyond the present to shape the future.
In a nutshell, collaboration has emerged as a critical “doorway” to positive outcomes in healthcare. If we want to achieve the triple aims of reform: 1) enhancing value; 2) improving the health of populations; and 3) reducing costs – collaboration is no longer optional.
While the doorway is now clearly visible, many in healthcare are struggling to get across the threshold to collaborate in new and innovative ways. Since emotional intelligence is a vital key to collaboration and these skills are learnable[7], if we want more collaboration in healthcare, it may be time for a concerted effort to cultivate and integrate these skills.
How are you contributing to positive change in health care through collaboration?
What makes your collaborations successful?
This article was a collaboration between Colette Herrick and Joshua Freedman.
References:
1 Javanmardian, M. Saxena, S.B. “Allies in Values-Based Care.” Trustee: 66:(5) May 2013, 13-16.
2 Nixon, A. A Note for Health Insurers Everywhere: Keep a Close Eye on Pittsburgh, Med City News: Today’s Headlines, www.medcitynews.com, July 29, 2013.
3 Institute of Medicine: Future of Nursing: Leading Change, Advancing Health, (2011), National Academies Press
4 Chrislip, David (2002). The Collaborative Leadership Fieldbook – A guide for citizens and civic leaders. Josey Bass.
5 Freedman, J. (2009) At the Heart of Leadership. Six-Seconds
6 Rock, David. (2006) Your Brain at Work. Harper-Collins
7 Fariselli, Freedman, Ghini (2006). White Paper: Increasing Emotional Intelligence (www.6seconds.org/tools/sei/research)
8 This sample consists of 321 healthcare professionals and senior managers from around the globe, from the SEI norm base in 2011-2012. SEI is a normed, validated assessment of emotional intelligence (www.6seconds.org/sei) Freedman, Jensen, Ghini (2005), The Six Seconds Emotional Intelligence Assessment.
- Enhance Emotional Literacy - July 13, 2023
- Plutchik’s Wheel of Emotions: Feelings Wheel - March 13, 2022
- Technology Loneliness: EQ Tips from Daniel Goleman - October 24, 2020

Hi Colette I’m Roberto Micarelli from Italy (Six Seconds PP and NL too) we’re focused as you on helping healthcare nurse and physician to live better and do a better job working with EQ, we’re going to plan a trial on a big campus in Italy and we would like some more news, presentation and data to let the management be more involved with the research. The Campus is Joint Commission Certified and has got some issue into a change management phase so we would like to plan a research and a trial to let people work better for them and for their patients. Be well and thanks in advance for your help Roberto.
Heather, thanks for your comments. As a nurse and survivor it sounds like you know first hand many of the pressures on providers. I like your suggestion of being the change you want to see and being optimistic with your healthcare providers. I remember when I practiced clinically and was not present or irritable, it was such a gift when a patient helped me to get back in touch with empathy… for myself and others!
Wow! So that’s whats wrong. (Sorry for the lack of optimism in that statement) As a nurse and a survivor of chronic pain, I have attempted an approach of Ahimsa or non-violence in my communication and have been met with everything from ambivalence to verbal brutality. What I see in this article is that the well-rigged defensiveness has been the groove turned rut of the medical/insurance culture.
Defective communication takes time, and it’s at a premium in the industry. Most people are rewarded for disengaging with their feeling in the work environment or health care field (which is one of the reasons burn-out is so high in the nursing culture). But the real hope here is optimism. That’s a place were most people, even time stretched emotion-suppressing people can get a foot in the door.
I will put optimism on the table, first, as I approach my health care providers.
After all, we must be the change we want to see in the world.
Sorry, that should be “effective communication” not “defective communication”. Oopsie.
Wonderful article, and well done to both of you. I’m a fan of ‘Tribal Leadership’, a book about stages of cultural development. Collaboration is the essence of a stage 4, honoring relationships and working in teams of three or more (‘triads’). As a hospital administrator, I must promote ‘weHealth’, and shift from a ‘me’ perspective. ‘We’ performance, working together, serves the patient better and changes the quality of our own lives, professionally and personally. Working within a larger community, where ‘healthcare’ is acknowledged as a spoke in the overall scheme of things, enhances engagement and facilitates even more collaboration.
What a Timely article for healthcare providers. In light of all the changes in healthcare these goals will be helpful moving forward.
Great to see an article that demonstrates, in the bio-physical language of healthcare professionals, the value of of emotional self awareness and collaboration!
Hello Colette and Josh – love the way you two collaborated to produce this compelling argument for emotional intelligence and collaboration in healthcare!
I was particularly glad to see your inclusion of the IOM’s recommendation that members of health care teams should partner with each other to redesign how health care looks.
Midwifery is likely the best example of how a once-contentious partnership has been slowly evolving (doctors have been among those most vehemently opposed to the legalization of midwifery). Here in Canada, midwives were first charged with practicing medicine without a license in 1981. But in 1993 (just 12 years later – that’s warp speed in medicine!) our British Columbia provincial government announced that midwifery would be legalized. Today, midwifery services in BC are completely funded through our health care system, referrals from a family physician or other practitioner are NOT necessary, and midwives can be contracted by expectant mothers for either home or hospital births. A number of published studies report that women assisted by midwives “have had a more positive attitude about their birth experience and are more satisfied with the care they received compared to that provided by physicians.”
Yet opposition to midwifery remains among many physicians in a kind of misguided turf war, often because of what some refer to as “cream-skimming” – the ability of midwives to siphon off billing for low-risk, non-complicated births.
One can only wonder when the emotional intelligence of physicians will kick in to collaborate in what’s clearly in the best interests of maternity patients.
Great article Colette and Joshua! While I’ve read quite a lot about emotional intelligence, I haven’t seen as much about the critical importance of collaboration or collaboration’s building block, namely, making a connection! So, thanks for the great piece and the practical tips about how to improve relationship-building and connecting with those we collaborate and work with on a daily basis.
Thanks for connecting, Doug!
My pleasure Colette! Thank you! I may reference your article in one of my future Hospital Impact blogs!
Absolutely:-)!
Excellent article. One of the major challenges to collaboration is the degree to which competition is rewarded. Institutions talk about valuing collaboration, but then ignore it or, often, view it as a negative for promotion. The traditional hierarchical nature of medicine is another challenge. Many physicians automatically discount suggestions coming from non-physicians. Much of this is based on ignorance of what non-physicians actually do during a workday. Inter-professional education will be crucial for long term success of collaborative approaches to health care. Finally, while I love optimism, excess optimism in the face of a major challenge can deflate the energy by seeming to imply that the work isn’t hard.
That’s a compelling, challenging point Harriet: If our systems continue to reward ‘winning over others’ then collaboration is a hard sell. We need to learn to evaluate & recognize (reward) meaningful collaboration.
BTW, re Optimism, at Six Seconds we often talk about ‘realistic optimism’: it doesn’t mean ‘pretending there’s no mess,’ it means ‘knowing there is a way out of the mess.’ 🙂
Exceptional article on collaboration!